ADAPTASI FISIOLOGIS BAYI BARU LAHIR
I. PERUBAHAN SISTEM PERNAFASAN
Perkembangan paru-paru
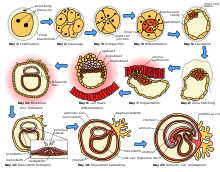
Paru-paru berasal dari titik tumbuh yang muncul dari pharynx, yang bercabang dan kemudian bercabang kembali membentuk struktur percabangan bronkus. Proses ini terus berlanjut setelah kelahiran hingga sekitar usia 8 tahun sampai jumlah bronkiolus dan alveolus akan sepenuhnya berkembang, walaupun janin memperlihatkan adanya bukti gerakan napas sepanjang trimester kedua dan ketiga (Varney’s, halaman 551). Ketidakmatangan paru-paru terutama akan mengurangi peluang kelangsungan hidup bayi baru lahir sebelum usia kehamilan 24 minggu, yang disebabkan oleh keterbatasan permukaan alveolus, ketidakmatangan system kapiler paru-paru dan tidak mencukupinya jumlah surfaktan.
Awal adanya nafas
Dua factor yang berperan pada rangsangan napas pertama bayi.
1. Hipoksia pada akhir persalinan dan rangsangan fisik lingkungan luar rahim yang merangsang pusat pernapasan di otak.
2. Tekanan terhadap rongga dada, yang terjadi karena kompresi paru-paru selama persalinan, yang merangsang masuknya udara kedalam paru-paru secara mekanis.
Interaksi antara system pernapasan, kardiovaskuler dan susunan saraf pusat menimbulkan pernapasan yang teratur dan berkesinambungan serta denyut yang diperlukan untuk kehidupan. Jadi system-sistem harus berfungsi secara normal.
Surfaktan dan upaya respirasi untuk bernafas
Upaya pernapasan pertama seorang bayi berfungsi untuk :
1. Mengeluarkan cairan dalam paru-paru
2. Mengembangkan jaringan alveolus paru-paru untuk pertama kali
Agar alveolus dapat berfungsi, harus terdapat surfaktan yang cukup dan aliran darah ke paru-paru. Produksi surfaktan dimulai pada 20 minggu kehamilan dan jumlahnya akan meningkat sampai paru-paru matang sekitar 30-34 minggu kehamilan. Surfaktan ini mengurangi tekanan permukaan paru dan membantu untuk menstabilkan dinding alveolus sehingga tidak kolaps pada akhir pernapasan
Tanpa surfaktan, alveoli akan kolaps setiap saat setelah akhir setiap pernapasan, yang menyebabkan sulit bernapas. Peningkatan kebutuhan energi ini memerlukan penggunaan lebih banyak oksigen dan glukosa. Peningkatan kebutuhan energi ini memerlukan penggunaan lebih banyak oksigen dan glukosa. Berbagai peningkatan ini menyebabkan stress pada bayi yang sebelumnya sudah terganggu.
Dari cairan menuju udara
Bayi cukup bulan, mempunyai cairan di dalam paru-parunya. Pada saat bayi melalui jalan lahir selama persalinan, sekitar sepertiga cairan ini diperas keluar dari paru-paru. Seorang bayi yang dilahirkan melalui seksio sesaria kehilangan keuntungan dari kompresi rongga dada ini dan dapat menderita paru-paru basah dalam jangka waktu lebih lama. Dengan beberapa kali tarikan napas pertama, udara memenuhi ruangan trakea dan bronkus bayi baru lahir. Dengan sisa cairan di dalam paru-paru dikeluarkan dari paru dan diserap oleh pembuluh limfe dan darah. Semua alveolus paru-paru akan berkembang terisi udara sesuai dengan perjalanan waktu.
Funsi system pernapasan dalam kaitanya dengan fungsi kardiovaskuler
Oksigenasi yang memadai merupakan factor yang sangat penting dalam mempertahankan kecukupan pertukaran udara. Jika terdapat hipoksia, pembuluh darah paru-paru akan mengalami vasokonstriksi. Pengerutan pembuluh ini berarti tidak ada pembuluh darah yang terbuka guna menerima oksigen yang berada dalam alveoli, sehingga menyebabkan penurunan oksigenasi jaringan, yang akan memperburuk hipoksia.
Peningkatan aliran darah paru-paru akan memperlancar pertukaran gas dalam alveolus dan menghilangkan cairan paru-paru. Peningkatan aliran darah ke paru-paru akan mendorong terjadinya peningkatan sirkulasi limfe dan membantu menghilangkan cairan paru-paru dan merangsang perubahan sirkulasi janin menjadi sirkulasi luar rahim.
II. PERUBAHAN SISTEM SIRKULASI
Setelah lahir, darah bayi baru lahir harus melewati paru untuk mengambil oksigen dan mengadakan sirkulasi melalui tubuh guna mengantarkan oksigen ke jaringan. Untuk membuat sirkulasi yang baik guna mendukung kehidupan luar rahim, harus terjadi dua perubahan besar:
1. Penutupan foramen ovale pada atrium jantung
2. Penutupan duktus arteriosus antara arteri paru-paru dan aorta.
Perubahan sirkulasi ini terjadi akibat perubahan tekanan pada seluruh system pembuluh tubuh. Ingat hokum yang menyatakan bahwa darah akan mengalir pada daerah-daerah yang mempunyai resistensi yang kecil. Jadi perubahan-perubahan tekanan langsung berpengaruh pada aliran darah.
Oksigen menyebabkan system pembuluh mengubah tekanan dengan cara mengurangi atau meningkatkan resistensinya, sehingga mengubah aliran darah. Hal ini terutama penting kalau kita ingt bahwa sebagian besar kematian dini bayi baru lahir berkaitan dengan oksigen (asfiksia).
Dua peristiwa yang mengubah tekanan dalam system pembuluh darah :
1. Pada saat tali pusat dipotong, resistensi pembuluh sistemik meningkat dan tekanan atrium kanan menurun. Tekanan atrium kanan menurun karena berkurangnya aliran darah ke atrium kanan tersebut. Hal ini menyebabkan penurunan volume dan tekanan atrium kanan itu sendiri. Kedua kejadian ini membantu darah dengan kandungan oksigen sedikit mengalir ke paru-paru untuk menjalani proses oksigenasi ulang.
2. Pernapasan pertama menurunkan resistensi pembuluh darah paru-paru dan meningkatkan tekanan atrium kanan. Oksigen pada pernapasan pertama ini menimbulkan relaksasi dan terbukanya system pembuluh darah paru-paru (menurunkan resistensi pembuluh darah paru-paru). Peningkatan sirkulasi ke paru-paru mengakibatkan peningkatan volume darah dan tekanan pada atrium kanan. Dengan peningkatan volume darah dan tekanan pada atrium kiri, foramen ovale secara fungsional akan menutup.
Vena umbilicus, duktus venosus dan arteri hipogastrika dari tali pusat menutup secara funsional dalam beberapa menit setelah lahir dan setelah tali pusat diklem. Penutupan anatomi jaringan fibrosa berlangsung dalam 2-3 bulan
III. PERUBAHAN SISTEM TERMOREGULASI
Bayi baru lahir belum dapat mengatur suhu tubuh mereka, sehingga akan mengalami stress dengan adanya perubahan-perubahan lingkungan. Pada saat bayi meninggalkan lingkungan rahim ibu yang hangat, bayi tersebut kemudian masuk ke dalam lingkungan ruang bersalin yang jauh lebih dingin. Suhu dingin ini menyebabkan air ketuban menguap lewat kulit, sehingga mendinginkan darah bayi.
Pada lingkungan yang dingin, pembentukan suhu tanpa mekanisme menggigil merupakan usaha utama seorang bayi yang kedinginan untuk mendapatkan kembali panas tubuhnya. Pembentukan suhu tanpa menggigil ini merupakan hasil penggunaan lemak coklat terdapat di seluruh tubuh, dan mereka mampu meningkatkan panas tubuh sampai 100 %. Untuk membakar lemak coklat, seorang bayi harus menggunakan glukosa guna mendapatkan energi yang akan mengubah lemak menjadi panas. Lemak coklat tidak dapat diproduksi ulang oleh bayi baru lahir dan cadangan lemak coklat ini akan habis dalam waktu singkat dengan adanya stress dingin. Semakin lama usia kehamilan, semakin banyak persediaan lemak coklat bayi.
Jika seorang bayi kedinginan, dia akan mulai mengalami hipoglikemia, hipoksia dan asidosis. Oleh karena itu, upaya pencegahan kehilangan panas merupakan prioritas utama dan bidan berkewajiban untuk meminimalkan kehilangan panas pada bayi baru lahir.
Disebut sebagai hipotermia bila suhu tubuh turun dibawah 360 C. Suhu normal pada neonatus adalah 36 5 – 370 C.
Bayi baru lahir mudah sekali terkena hipotermia yang disebabkan oleh:
1. Pusat pengaturan suhu tubuh pada bayi belum berfungsi dengan sempurna
2. Permukaan tubuh bayi relative lebih luas
3. Tubuh bayi terlalu kecil untuk memproduksi dan menyimpan panas
4. Bayi belum mampu mengatur possisi tubuh dan pakaiannya agar ia tidak kedinginan.
Hipotermia dapat terjadi setiap saat apabila suhu disekeliling bayi rendah dan upaya mempertahankan suhu tubuh tidak diterapkan secara tepat, terutama pada masa stabilisasi yaitu 6 – 12 jam pertama setelah lahir. Misal: bayi baru lahir dibiarkan basah dan telanjang selama menunggu plasenta lahir atau meskipun lingkungan disekitar bayi cukup hangat namun bayi dibiarkan telanjang atau segera dimandikan.
Gejala hipotermia:
1. Sejalan dengan menurunnya suhu tubuh, bayi menjadi kurang aktif, letargis, hipotonus, tidak kuat menghisap ASI dan menangis lemah.
2. Pernapasan megap-megap dan lambat, denyut jantung menurun.
3. Timbul sklerema : kulit mengeras berwarna kemerahan terutama dibagian punggung, tungkai dan lengan.
4. Muka bayi berwarna merah terang
5. Hipotermia menyebabkan terjadinya perubahan metabolisme tubuh yang akan berakhir dengan kegagalan fungsi jantung, perdarahan terutama pada paru-paru, ikterus dan kematian.
Mekanisme terjadinya Hipotermia:
Hipotermia pada bayi baru lahir timbul karena penurunan suhu tubuh yang dapat terjadi melalui:
1. Radiasi : Yaitu panas tubuh bayi memancar kelingkungan sekitar bayi yang lebih dingin, misal : BBL diletakkan ditempat yang dingin.
2. Evaporasi : Yaitu cairan/air ketuban yang membasahi kulit bayi menguap, misal : BBL tidak langsung dikeringkan dari air ketuban.
3. Konduksi : Yaitu pindahnya panas tubuh bayi karena kulit bayi langsung kontak dengan permukaan yang lebih dingin, misal : popok/celana basah tidak langsung diganti.
4. Konveksi : Yaitu hilangnya panas tubuh bayi karena aliran udara sekeliling bayi, misal : BBL diletakkan dekat pintu/jendela terbuka.
IV. PERUBAHAN SISTEM METABOLISME
Untuk memfungsikan otak memerlukan glukosa dalam jumlah tertentu. Dengan tindakan penjepitan tali pusat dengan klem pada saat lahir seorang bayi harus mulai mempertahankan kadar glukosa darahnya sendiri. Pada setiap baru lahir, glukosa darah akan turun dalam waktu cepat (1 sampai 2 jam).
Koreksi penurunan gula darah dapat dilakukan dengan 3 cara :
1. Melalui penggunaan ASI (bayi baru lahir sehat harus didorong untuk menyusu ASI secepat mungkin setelah lahir).
2. Melalui penggunaan cadangan glikogen (glikogenesis)
3. Melalui pembuatan glukosa dari sumber lain terutama lemak (glukoneogenesis).
Bayi baru lahir yang tidak dapat mencerna makanan dalam jumlah yang cukup akan membuat glukosa dari glikogen (glikogenolisis). Hal ini hanya terjadi jika bayi mempunyai persediaan glikogen yang cukup. Seorang bayi yang sehat akan menyimpan glukosa sebagai glikogen, terutama dalam hati, selama bulan-bulan terakhir kehidupan dalam rahim. Seorang bayi yang mengalami hipotermia pada saat lahir yang mengakibatkan hipoksia akan menggunakan persediaan glikogen dalam jam pertama kelahiran. Inilah sebabnya mengapa sangat penting menjaga semua bayi dalam keadaan hangat. Perhatikan bahwa keseimbangan glukosa tidak sepenuhnya tercapai hingga 3-4 jam pertama pada bayi cukup bulan yang sehat. Jika semua persediaan digunakan pada jam pertama maka otak bayi dalam keadaan beresiko. Bayi baru lahir kurang bulan, lewat bulan, hambatan pertumbuhan dalam rahim dan distress janin merupakan resiko utama, karena simpanan energi berkurang atau digunakan sebelum lahir.
Gejala-gejala hipoglikemia bisa tidak jelas dan tidak khas meliputi : kejang-kejang halus, sianosis, apnu, tangis lemah, letargis, lunglai dan menolak makanan. Bidan harus selalu ingat bahwa hipoglikemia dapat tanpa gejala pada awalnya. Akibat jangka panjang hipoglikemia ialah kerusakan yang meluas di seluruh sel-sel otak.
V. PERUBAHAN SISTEM GASTROINTESTINAL
Sebelum lahir, janin cukup bulan akan mulai menghisap dan menelan. Refleks gumoh dan refleks batuk yang matang sudah terbentuk dengan baik pada saat lahir.
Kemampuan bayi baru lahir cukup bulan untuk menelan dan mencerna makanan (selain susu) masih terbatas. Hubungan antara esophagus bawah dan lambung masih belum sempurna yang mengakibatkan “gumoh” pada bayi baru lahir dan neonatus. Kapasitas lambung sendiri sangat terbatas, kurang dari 30 cc untuk seorang bayi baru lahir cukup bulan. Kapasitas lambung ini akan bertambah secara lambat bersamaan dengan tumbuhnya bayi baru lahir. Pengaturan makan yang sering oleh bayi sendiri penting contohnya memeberi ASI on demand.
Usus bayi masih belum matang sehingga tidak mampu melindungi dirinya sendiri dari zat-zat berbahaya kolon. Pada bayi baru lahir kurang efisien dalam mempertahankan air disbanding orang dewasa, sehingga menyebabkan diare yang lebih serius pada neonatus.
VI. PERUBAHAN SISTEM KEKEBALAN TUBUH
Sistem imunitas bayi baru lahir masih belum matang, sehingga menyebabkan neonatus rentan terhadap berbagai infeksi dan alergi. Sistem imunitas yang matang akan memberikan kekebalan alami maupun yang didapat.
Kekebalan alami terdiri dari struktur pertahanan tubuh yang mencegah atau meminimalkan infeksi. Berikut beberapa contoh kekebalan alami meliputi:
1. Perlindungan oleh kulit membrane mukosa.
2. Fungsi saringan saluran napas.
3. Pembentukan koloni mikroba oleh kulit dan usus
4. Perlindungan kimia oleh lingkungan asam lambung.
Kekebalan alami juga disediakan pada tingkat sel oleh sel darah yang membantu bayi baru lahir membunuh mikroorganisme asing. Tetapi pada bayi baru lahir sel-sel darah ini masih belum matang, artinya bayi baru lahir tersebut belum mampu melokalisasi dan memerangi infeksi secara efisien.
Kekebalan yang didapat akan muncul kemudian. Bayi baru lahir yang lahir dengan kekebalan pasif mengandung banyak virus dalam tubuh ibunya. Reaksi antibody keseluruhan terhadap antigen asing masih belum bisa dilakukan sampai awal kehidupan anak. Salah satu tuges utama selama masa bayi dan balita adalah pembentukan system kekebalan tubuh.
Karena adanya defisiensi kekebalan alami dan didapat ini, bayi baru lahir sangat rentan terhadap infeksi. Reaksi bayi baru lahir terhadap infeksi masih lemah dan tidak memadai. Oleh karena itu, pencegahan terhadap mikroba (seperti pada praktek persalinan yang aman dan menyusui ASI dini terutama kolostrum) dan detekdi dini serta pengobatan dini infeksi menjadi sangat penting.